With the passage of the federal parity law, along with the Affordable Care Act and the decision by 32 states (including the District of Columbia) to expand Medicaid, Americans should have better access to mental health care than at any time in history. Yet, people with mental health conditions who have insurance still struggle to find providers and services in their networks.
The majority of the mental health professionals in my area do not participate in any insurance plans. The in-network providers do not have the same level of quality. My insurance plan has an $8,000 deductible for out of network benefits. The psychiatrist charges $215 and the insurance reimburses $60… We have depleted our savings and incurred much debt to get the quality mental health care we need..
One reason for the difficulty finding in-network mental health care is the critical nationwide shortage of mental health professionals.
[My relative] has had terrible trouble finding a psychiatrist in our community. He has been traveling 50 miles each way to see a psychiatrist. The wait lists for all psychiatrists locally are for between 6 months and two years.
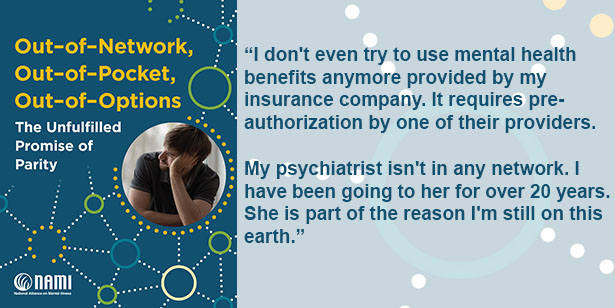
Adding to the problem, many mental health providers—particularly psychiatrists—are not in health plan networks.
I have a psychiatrist who also handles my psychotherapy. Insurance will only reimburse him $75 for an hour of services. He is out of network – he has to be – at $225 an hour. My current insurance has no deductible limit on out of network services. I have to pay 100% and have had to cut back on psychiatry visits. This has caused a lot of problems and threatens my ability to maintain my job.
Mental health providers often cite low reimbursement rates and heavy administrative burden as the main reasons they have chosen not to participate in health plan networks. Meanwhile, people seeking care have difficulty finding accurate information about participating mental health professionals in their health insurance plans. On top of that, frequent changes in health plan provider networks leads to disruptions in care, confusion and unexpected medical bills for consumers.
In April 2015, NAMI issued a report, A Long Road Ahead: Achieving True Parity in Mental Health and Substance Use Care, which described the results of a survey conducted in the winter of 2014 on the experiences of people with mental health conditions and their families with private health insurance. The survey revealed that, despite the requirements of the federal parity law, people encountered significant barriers to receiving services.
In Mental Health Parity & Network Adequacy, NAMI highlights the findings of its most recent survey results, which echo the same truth about the status of mental health parity that we found in 2015: we’re not there yet.
To follow-up on the findings published in early 2015, NAMI conducted an online survey in the winter of 2015 to answer the question, “What do insurance beneficiaries experience when they seek mental health care?” The survey drew responses from 3,081 individuals and found that people with insurance had more difficulty locating in-network providers and facilities for mental health care compared to general or specialty medical care. This was true of both inpatient mental health care and outpatient mental health care.
Survey results showed that people were far less likely to find or use an in-network mental health provider compared to other types of medical specialists.

Survey respondents were also more likely to go out-of-network and incur high expenses for psychiatric hospital care and psychiatric residential treatment than for hospital care to treat other medical conditions.

Survey respondents faced greater out-of-pocket costs (costs not covered by insurance) for outpatient and inpatient mental health care than for other types of specialty medical care. Out-of-pocket costs were significantly higher for both mental health prescribers and therapists compared to medical specialty care.

Eight in ten respondents had out-of-pocket costs of over $200 for psychiatric hospital or residential mental health care compared to fewer than six in ten for general hospital care.

Medicaid recipients were more likely to have an in-network mental health prescriber or therapist than those with private insurance. Medicaid recipients were also more likely to use an in-network psychiatric hospital or residential treatment versus out-of-network facilities.
| Provider or Service | Medicaid In-Network Rate | Private Insurance In-Network Rate |
| Mental health prescriber | 86% | 70% |
| Mental health therapist | 82% | 68% |
| Psychiatric Hospital | 88% | 80% |
| Residential Mental Health | 80% | 57% |
NAMI recommends that insurance companies be required to take the following steps to improve coverage under federal parity law:
Despite the federal parity law, the promise of parity remains elusive. Consumers continue to face significant challenges finding a provider, getting an appointment and paying the bill for mental health care compared to other types of specialty medical care. For the sake of millions of children and adults affected by mental health conditions, NAMI calls on health plans—and state and federal lawmakers—to address these disparities and improve access to quality, affordable mental health care.
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264,
text “NAMI” to 62640, or email. In a crisis, call or text 988 (24/7).